Amanda Northrop/Vox
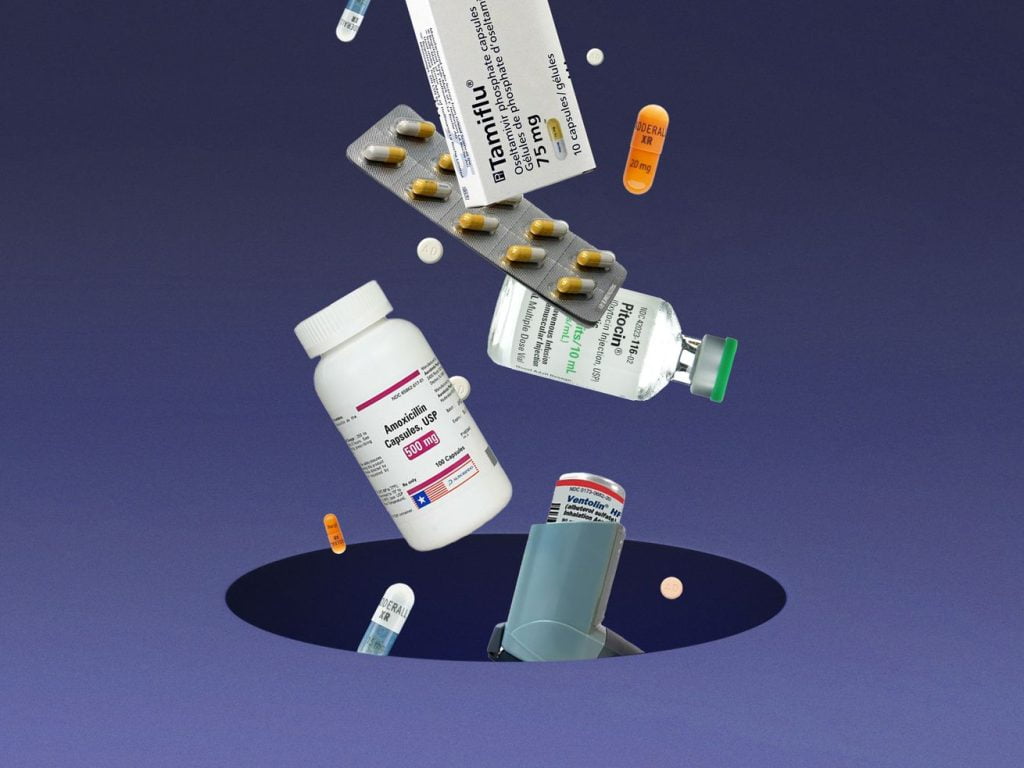
America’s frequent drug shortages put patients’ health — and their lives — at risk.
The United States, the world’s richest country and its most important developer of pharmaceuticals, is not supposed to run out of prescription drugs. And yet it does — all the time.
Just in the past few weeks, there have been reported shortages of amoxicillin and tamiflu in the midst of a surge in respiratory infections. Young patients with asthma who contract the respiratory syncytial virus (RSV) might need albuterol to ameliorate breathing problems, but that medication has been in short supply for months.
Shortages of drugs to treat all kinds of conditions are happening across the health system. There is an ongoing shortage of Adderall. Shortages of saline, morphine, and cancer drugs have occurred in recent years. When Covid-19 arrived in the United States two years ago, the country was already short on the drugs necessary for people placed on ventilators. And when I learned two months ago about shortages of Pitocin, the medication used to induce labor as well as to control bleeding from postnatal hemorrhages, Mark Turrentine, an OB-GYN at the Baylor College of Medicine, told me that these localized Pitocin shortages were “not something that happened just recently” but they had occurred repeatedly “over the past four or five years.”
According to a 2022 report from the National Academies of Sciences, Engineering, and Medicine, “on average, the number of ongoing drug shortages has been increasing and are lasting longer.” The root cause of that problem, per a report from the Food and Drug Administration, is the economics of the pharmaceutical market itself.
The reasons for shortages are generally consistent no matter the drug: either a shortage of raw materials or a problem at the plant where the drug is manufactured. Shortages for medicines that a patient can pick up at the pharmacy often draw the most headlines, but most of the medications that end up in short supply are generic, injectable drugs that are used in hospitals: usually, these drugs have only one or two suppliers. So if there is a problem at the factory of one company, there is not an easy way to scale up production to make up for a shortfall. And they are usually cheap, which means the companies that manufacture them do not have a strong economic incentive to produce any excess supply.
“We haven’t invested in expanding the capacity our country needs. It’s costly. If you’re going to sell something for a dollar a vial, there’s no incentive to invest there,” said Erin Fox, a pharmacist at the University of Utah who has studied drug shortages. “It makes a lot of sense when you think about it from their perspective. But when you think about it from the hospital perspective, it’s very frustrating.”
Some of these shortages have led directly to patient deaths. An Associated Press report in 2011 linked at least 15 deaths over the prior 15 months to drug shortages. A more recent study, following the year-long shortage of a drug used to treat septic shock, found higher mortality rates for patients who relied on a substitute. Even short of death, drug shortages can meaningfully change the care patients get — if, for example, a pregnant person undergoes a cesarean delivery, with its higher risk of complications and longer recovery time, because the drug that could have induced labor earlier is out of stock.
Experts do have ideas about how to make the pharmaceutical supply chain more resilient. But they require action by the federal government. Until that happens, there is little reason to think the pace and duration of America’s drug shortages will slow down.
Why drug shortages happen — and their sometimes deadly consequences
Manufacturing a prescription drug is complicated. A company first has to acquire the necessary ingredients, sometimes from suppliers all over the world. The producer must take those raw materials and then manufacture the drug, at a factory capable of executing a technically sophisticated production process, in the most economical fashion, while also meeting FDA safety and quality requirements.
Take a look at this graphic from the National Academies report. Every drug on the market has its own variation of this flow chart.
NASEM
Most shortages can be traced to a lack of raw materials or, most often, a problem at the manufacturing site. Machines break. Ingredients get contaminated. Manufacturers are not required to disclose the reasons for a shortage, but the recent shortage of baby formula — while it’s not a drug — is illustrative. The FDA required Abbott Nutrition, one of the largest suppliers of baby formula, to shut down its main plant because of unsanitary conditions and contaminated products.
As with the baby formula shortage, it’s hard for the industry to compensate when production is halted. Most of the drugs that experience shortages are generics, and there are generally only a handful of companies producing a given generic drug. If one of them has production problems, it can mean that suddenly half — or more — of the expected supply is wiped out.
And once the supply is disrupted, it’s impossible to quickly make up for the shortfall. These companies rely on razor-thin margins and massive scale to make their business work. They have a “just in time” production schedule, which means almost as soon as the product rolls out of the factory, it is delivered to health care providers. There aren’t warehouses with emergency stockpiles, because it wouldn’t really make financial sense for manufacturers to produce and store the excess supply.
Shortages due to distribution problems or an increase in demand are less common, but they do happen. Fox pointed to a looming strike of rail workers as one way that, even if a drug has been produced without problems, there can be a delay in getting it to patients. And in the early weeks of the pandemic, there was a surge in demand for drugs, including albuterol, that created temporary shortages.
Whatever the reason, shortages can have serious consequences. In 2011, there was a year-long shortage of norepinephrine, a blood pressure drug used for patients experiencing septic shock, because of production problems at three manufacturing sites. Researchers later compared the mortality rates of patients who needed norepinephrine for septic shock at hospitals that were out of the drug and relied on a substitute versus those treated at hospitals that still had it in supply. They found that patients at the facilities experiencing a shortage had a higher mortality rate.
The same applies for patients who need a longer treatment but can’t find the drug that would best serve them. One study found that the mortality rates among cancer patients who must use a substitute drug are higher. Replacing drugs can be difficult for clinicians; hospitals experiencing morphine and sedative shortages have reported patients being given the wrong dosage of a substitute drug, leading to serious clinical distress and even deaths.
But even if the stakes are not life and death, drug shortages can meaningfully change the kind of care patients receive. When I spoke with Turrentine about the Pitocin shortage, he said doctors may not be able to induce labor in a pregnant person without the drug, which increases the possibility of the patient needing a C-section delivery. C-sections are more invasive than vaginal childbirth, with a greater risk of complications and a longer recovery time. It ends up being more burdensome for the patient, and it costs more money to provide the care.
But the existence of these clinical consequences isn’t enough to force drugmakers to change their process or to start producing an excess supply. They are running a business, and the economics of drug production are driving these shortages. Those are not going to change unless policymakers overhaul the rules.
What the US could do to prevent future drug shortages
The authors of the National Academies report recommended several actions the federal government could take to address drug shortages, from trade agreements that make it easier to import and export medicines in a shortage to an overhaul of the National Strategic Stockpile, one of the few available reserves for a small number of essential drugs when there is not enough supply.
There are some other, shorter-term patches included in that list of recommendations that would make it possible to end a shortage sooner. Hospital systems could enter emergency purchasing agreements for certain vital products, to give them another option if their main supplier has a production problem. The government could do more to secure excess supply of some essential medicines as well.
Under the current system, though, it isn’t practical for the government to purchase excess supply of every possible pharmaceutical, nor does it make economic sense for the drug manufacturer to maintain reserves indefinitely. These solutions are really Band-Aids, deployed once there is already a shortage.
But how do we stop shortages from happening in the first place?
I asked Fox, one of the report’s authors, what she would prioritize if she had the opportunity to wave a magic wand and do one thing on drug shortages. Her answer: unlocking other possible solutions starts with more transparency.
Fox and her co-authors want pharmaceutical manufacturers to disclose more information about their production facilities and the ingredients they use to make drugs. That would help government officials identify potential vulnerabilities in the supply chain and better anticipate oncoming shortages if there is a breakdown in supply of those materials. Beyond that, though, they are also urging the FDA to make public its assessments of the safety of drug manufacturing plants and the quality (as in purity) of the medications produced there.
With that information, Fox envisions the creation of a rating system that would let both providers and patients know much more about where their drugs are coming from. That would allow them to make more informed decisions about which drugs to buy.
But higher-quality medicines are more expensive to make and therefore may cost more. So if hospitals are still making economic decisions to prioritize cost over quality, the feds could give them a nudge, Fox said. There could be carrots (such as tax credits for buying drugs from a higher-graded manufacturer) as well as sticks (making the purchase of drugs from a supplier with a certain rating or higher a condition of Medicaid or Medicare funding).
You could imagine a scenario in which steering purchasers toward certain products could lead to even more dependence on one supplier. But Fox’s response, when I raised that point, was that many products are already facing that situation, given the way the pharmaceutical market is constructed. At least under a system like she described, manufacturers would be rewarded for taking the steps that should make shortages less likely.
“There’s no profit for companies to invest in quality in manufacturing plants,” she said. A concept like this would be one way to change that. “Target our dollars to companies that are doing a good job.”
And even if higher-quality drugs mean more expensive drugs, Fox argued that could still be a deal worth making. Drug shortages already drive up costs in subtler ways: Labor costs go up if patients are in the hospital longer and require more intensive care. A substitute drug might need to be bought, another expense. The clinical benefits should be obvious, given what we know about how shortages can negatively affect care.
Those are changes that won’t happen overnight, and they would require a serious commitment from the government. But Fox hopes the US sees an opportunity, given the way Covid-19 has made everyone more aware of and sensitive to supply chain problems of all kinds. It’s not always been easy to get policymakers to pay attention to drug shortages, she said. “It’s kind of a boring story. If there is a bright point to Covid, it’s shining a light to these supply chain problems.”
Until officials actually act, there are bound to be more shortages and more headlines like we have seen in the past few weeks. The problem is only getting worse.